Finding the right moment to bring your child to a developmental pediatrician can feel like trying to catch a comet—timing is everything, but the stakes are high. In this article we’ll break down the signs, the timing, and the process, all while keeping the tone light enough to keep you from pulling your hair out. Whether you’re a first‑time parent or a seasoned caregiver, you’ll walk away with clear next steps and a few chuckles along the way.
Understanding the Early Signs
Social Cues That Might Raise a Flag
- Limited eye contact during play or conversation Unusual response to their own name Difficulty sharing excitement (e.g., not pointing at a toy when you point at it)
These behaviors can appear in many children, but when they cluster, it’s worth paying attention. Think of them as the “red lights” on a road trip; they’re not always a stop sign, but they do warrant a closer look.
Communication Patterns Worth Noting
- Delayed first words beyond 16 months Repetitive speech (e.g., echoing phrases) A sudden drop in language use after an initial burst
If you notice a pattern, ask yourself: Could this be more than just a phase? The answer isn’t always obvious, but it’s a good starting point for conversation with your pediatrician.
Sensory Sensitivities
- Over‑reacting to lights, sounds, or textures Seeking out specific sensory experiences (e.g., spinning or staring at lights)
These sensitivities can be subtle or dramatic. Even if your child is just “quirky,” a pattern of avoidance or fixation can signal something deeper.
When to Reach Out: Timing Matters
The 18‑Month Check‑In
Many pediatricians schedule a developmental screening at 18 months. If your child hasn’t met milestones in social interaction, language, or motor skills, this is a natural point to discuss concerns. A developmental pediatrician can provide a more in‑depth assessment than a routine well‑child visit.

> “Early intervention is like planting a seed before winter; the sooner you nurture it, the stronger it grows.” – Dr. L. Patel, developmental specialist
A Quick Question: Do I Need a Formal Diagnosis Now?
Not necessarily. A developmental pediatrician can offer a diagnostic evaluation or simply a screening to identify areas that need support. The key is to avoid waiting until the child is older, as early services can make a measurable difference.
Signs That Demand Immediate Attention
- Significant regression in speech or motor skills Severe tantrums or meltdowns that disrupt daily life Safety concerns (e.g., running into traffic, swallowing small objects)
If any of these appear, schedule an appointment promptly—time is a powerful ally in early intervention.
Choosing the Right Specialist
Credentials That Matter
- Board‑certified in developmental pediatrics Experience with autism spectrum disorders (ASD) Familiarity with the latest diagnostic criteria (DSM‑5)
A quick Google search or a call to your local hospital can confirm these qualifications.
Personal Fit
- Communication style: Do they explain things clearly? Availability: Are they accessible for follow‑ups? Cultural sensitivity: Do they respect your family’s values and background?
You’ll be partnering with this professional for months, so trust and comfort are essential.
Asking the Right Questions
- What diagnostic tools do you use? How do you collaborate with schools and therapists? What support resources do you recommend?
A good developmental pediatrician will welcome these questions and provide transparent answers.
What to Expect During the Evaluation
The Assessment Process
Parent Interview – Your observations, concerns, and child history Direct Observation – Play sessions, social interactions, and sensory responses Standardized Tests – Language, cognitive, and adaptive behavior scales The entire evaluation usually takes 2–3 hours, but you’ll get a comprehensive picture of your child’s strengths and challenges.The Diagnosis (If Applicable)
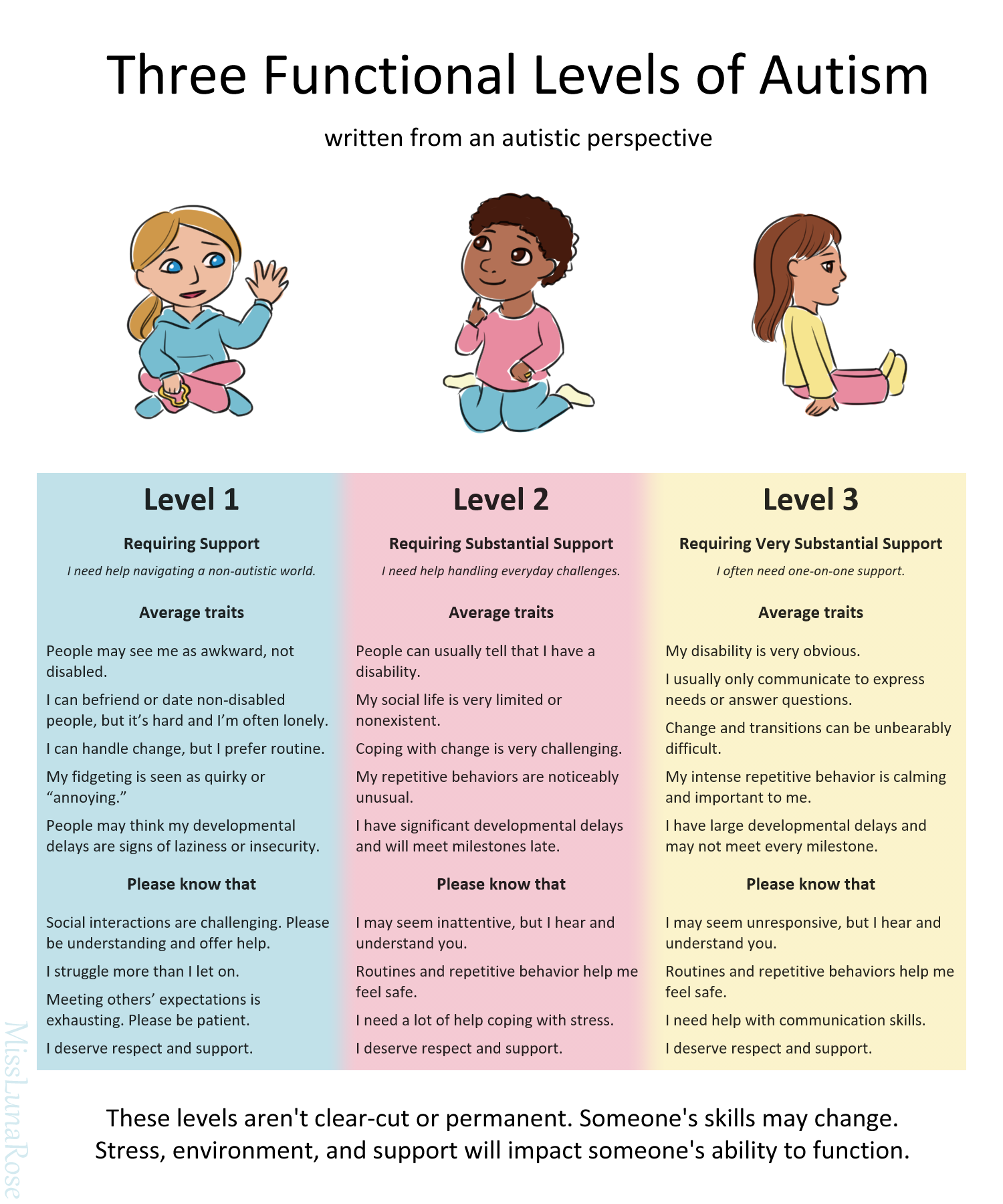
- Autism Spectrum Disorder (ASD) – May be labeled as high‑functioning or low‑functioning based on cognitive level Other developmental concerns – Such as language delay or sensory processing disorder
A diagnosis is not a verdict; it’s a roadmap to targeted support.
After the Evaluation
You’ll receive a written report and a meeting to discuss findings. This is also the time to ask about next steps: therapy options, school accommodations, and community resources.
Building a Supportive Team
Who Should Be Involved?
- Developmental pediatrician – The clinical guide Speech‑language pathologist – For communication challenges Occupational therapist – To address sensory and daily living skills Behavioral therapist – For strategies like Applied Behavior Analysis (ABA) School counselor – To coordinate educational support
Think of this team as Additional resources a sports squad: each member has a unique skill set, and together they aim Additional hints for the same championship—your child’s well‑being.
The Role of Family
Parents and siblings are often the most consistent caregivers. Providing them with training and resources can amplify the effectiveness of professional interventions.
Community Resources
- Parent support groups – Peer advice and shared experiences Local autism advocacy organizations – Information on funding and services Online forums – A place to ask questions and find tips
These networks can be lifesavers, especially when navigating insurance or finding specialized therapies.
Next Steps After the Diagnosis
Early Intervention Programs
Many states offer funded early intervention services for children under 3. These may include:
- Individualized Family Service Plans (IFSP) Therapeutic sessions (speech, occupational, behavioral) Parent training workshops
Enrollment is usually a matter of paperwork and a short waiting list.
Setting Goals
Work with your pediatrician and therapists to set realistic, measurable goals. Examples:
- Increase conversational turn‑taking by 50% in 6 months Reduce sensory‑triggered meltdowns to once a week Improve fine‑motor skills for self‑feeding
Tracking progress keeps everyone motivated and focused.
Advocating for Your Child
- Know your child’s rights (e.g., IDEA, ADA) Document milestones and setbacks Communicate regularly with educators
Advocacy is a marathon, not a sprint. A clear, organized approach yields the best outcomes.
Making Your Selection Count
Choosing a developmental pediatrician is a pivotal decision that can shape your child’s trajectory. Keep these final pointers in mind:
- Trust your instincts – If something feels off, explore other options. Look for a collaborative approach – A specialist who works with therapists, schools, and families is gold. Prioritize accessibility – Proximity, appointment flexibility, and insurance coverage matter.
Remember, the goal isn’t just a diagnosis; it’s a partnership that empowers your child to thrive. If you’re ready to take the next step, schedule a consultation today. Your child’s future is a bright canvas—let a skilled developmental pediatrician help you paint it with confidence and care.